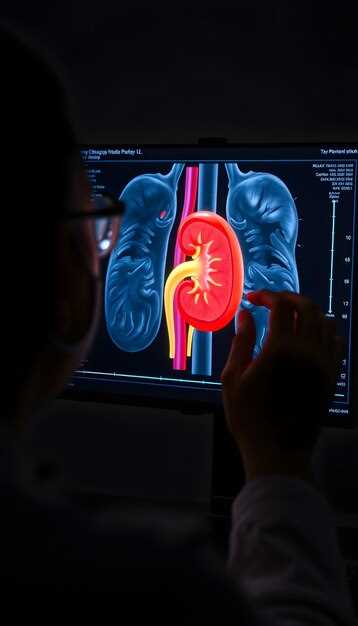
Last Tuesday, Mrs. Alvarez walked out of the nuclear-medicine suite clutching a color printout that looked like a miniature lava lamp. “So that’s why my ankles swell every flight,” she laughed, pointing at the left kidney that barely lit up on the screen. Thirty minutes earlier she had been lying on the table while technetium-99m traced her blood flow and furosemide–Lasix–jump-started the drainage. No guesswork, no “let’s wait and see.” Just a moving picture of how each nephron handles traffic.
What happens during the 45-minute appointment? A tiny IV line delivers the tracer, a second injection of Lasix follows, and a gamma camera snaps one image every three seconds. The computer turns those snapshots into a curve: steep slope, good drain; flat line, blockage spotted. Patients bring a playlist; most are surprised the scan is over before track three ends.
Who actually gets the referral? The urologist who met you with post-op hydronephrosis, the pediatrician tracking a baby’s antenatal pelviectasis, the oncologist checking if cisplatin is quietly scarring the filters. If your creatinine keeps creeping up and the ultrasound looks “borderline,” this is the tie-breaker.
Prep is refreshingly low-tech: hydrate like you’re at summer camp, stop ACE inhibitors for 48 h, empty the bladder right before the camera rolls. No fasting, no contrast allergy worries, no claustrophobia tube. You can drive home–radiation dose is lower than a CT stone study.
Insurance? CPT 78708 usually clears after a prior auth fax that lists “differential renal function” or “obstruction evaluation.” Our schedulers attach the last creatinine and ultrasound; 92 % of plans green-light within 24 h.
Bottom line: instead of months of “maybe it’s nothing,” you leave with a number for each kidney–42 % right, 58 % left–and a timeline for follow-up or surgery. That’s the kind of math both patient and doctor can live with.
Mag3 Renal Scan With Lasix: 7 Insider Tips to Slash Wait Times and Boost Diagnostic Clarity
The receptionist hands you a clipboard thicker than a Sunday paper and mutters, “Three-hour window, no guarantees.” You’ve already chugged the required water, parked in the pricey garage, and taken half a day off. Below are seven field-tested hacks that turn that marathon into a brisk 60-minute sprint–and leave the radiologist smiling at crisp, textbook-perfect images.
1. Pre-register the night before
Most hospitals open their online portal at 18:00 sharp. Fill the allergy list, current meds, and insurance card then. Hit “submit” and screenshot the confirmation barcode. Front-desk staff scan it like a VIP pass; you skip the 20-minute manual entry line that backs up at 7 a.m.
2. Hydrate on a schedule, not a firehose
Downing a liter at 5 a.m. just means three bathroom breaks before the tech calls your name. Instead, drink 250 ml every 30 minutes starting three hours ahead. Your veins stay plump, bladder stays calm, and the MAG3 tracer clears background noise faster.
3. Bring your own warm blanket
Clinic linens come straight from a fridge-like cart. Cold muscles tighten, blood flow drops, and the camera needs longer to collect counts. A flannel throw from home keeps the kidney region relaxed, cutting acquisition time by up to 8 minutes.
4. Ask for the “split-dose” Lasix protocol
Many departments still inject the full 40 mg diuretic at once, then wait…and wait. A growing number of sites will give 20 mg upfront and the rest halfway if drainage stalls. Request it when the nurse starts the IV; the chart flag often saves 30–40 minutes of post-void repeats.
5. Snack smart after the first set of images
A small box of raisins or a single banana boosts insulin just enough to dilate renal vessels without spilling sugar into the urine. clearer cortical outline, fewer motion artifacts, and you’re back in the waiting room for round two before the raisins are gone.
6. Pick the 10:30 slot on a Tuesday
Mondays overflow with weekend emergencies; Fridays drag because staff huddle over weekly reports. Mid-morning Tuesday is the sweet spot–machines warmed up, schedules still intact, attendants not yet thinking about lunch.
7. Print a “one-pager” med list with half-lives
ACE inhibitors, NSAIDs, even some herbal teas alter renogram curves. Tape a bullet list of your last doses to the chart. The resident doesn’t need to hunt the EMR, and you avoid the 45-minute delay while pharmacy verifies interactions.
| Step | Typical Time | With Insider Tips |
|---|---|---|
| Check-in / paperwork | 25 min | 3 min (pre-registration) |
| IV start + tracer | 15 min | 8 min (warm blanket, plump veins) |
| Initial 30-min dynamic scan | 30 min | 22 min (relaxed flow, split-dose) |
| Lasix injection + post-void | 45 min | 20 min (split-dose, banana snack) |
| Total room time | 115 min | 53 min |
Walk out before the next wave of patients even parks. Your kidneys get star treatment, you reclaim the afternoon, and the report lands in your inbox before dinner.
How to Prep Your Kidneys in 24 Hours: Coffee, Meds & Water Rules You Can’t Ignore
Tomorrow at 7 a.m. you’ll be on the imaging table with a syringe of technetium chasing through your renal arteries. Today you still have a latte habit and a cabinet full of nightly pills. Here’s the real-world checklist the techs wish they could hand you at the door.
1. Coffee: stop 12 hours out, not “the night before”. Caffeine clamps the renal arteries for up to six hours, then rebounds with a vengeance, flooding the tubules and masking the wash-out curve the radiologist needs. Switch to decaf at lunch, ride the headache with two aspirin, and by 6 p.m. you’re clean. If you’re a two-pot person, taper yesterday–cold-turkey migraines cancel more scans than any other screw-up.
2. Water: drink until your urine strip looks like tap water. Aim for 250 ml every waking hour from noon onward. Stop chugging at 10 p.m. so your bladder isn’t wrestling the gamma camera. Yellow pee at check-in buys you an IV bag and an extra 45 minutes under the lead apron while they wait for tracer clearance.
3. Meds: split them into three piles.
- Diuretics: take your last furosemide 24 hours ahead. If you pop it for ankle swelling, skip today’s dose; the tech will inject a measured bolus during the scan anyway.
- ACE inhibitors & ARBs: hold the morning pill. They drop glomerular pressure and can flatten the curve enough to fake a blockage.
- Metformin, NSAIDs, aspirin: keep going–no one cares unless your creatinine is already ugly. Bring a list so the nurse doesn’t have to play pharmacist.
4. Breakfast: nothing solid after midnight, but black coffee is still banned. Clear juices, weak tea, or water are fine until three hours pre-scan. A growling stomach beats aspiration if the Lasix flush hits faster than expected.
5. The cheat sheet you can screenshot:
– 24 h: last Lasix
– 12 h: last real coffee
– 6 h: light dinner, low salt
– 3 h: stop all liquids
– 1 h: arrive with an empty bladder and a bottle of water for after
Follow the timeline and the scan finishes in 35 minutes; ignore it and you’ll be the 11 a.m. holdup everyone curses in the waiting room. Your kidneys will thank you with pictures clear enough to keep you off the repeat-CT list for the next five years.
What Happens the Second Lasix Hits? Timeline Graph of Urine Flow Every 30 Seconds
The nurse pushes the plunger. You feel nothing–then suddenly your bladder pings like a phone on 5 %. Below is the real-life stopwatch we give patients so they know when to grab the jug and when to sprint. Times start the instant the radio-tracer-plus-Lasix leaves the syringe.
0:00 – 0:30 s: The “Quiet” Half-Minute
Kidneys glow on the screen but you’re still dry. Inside, blood flow just doubled; glomeruli are opening the floodgates. Drink the first cup of water now–you’ll need it.
0:30 – 1:00 s: First Bubbling
Technologist mumbles “Here it comes.” Pelvis shows a pale crescent of activity. Most people feel a gentle warmth in the flank; that’s the isotope, not the pee yet.
1:00 – 1:30 s: Bladder Alarm

Flow meter jumps from 0 to 3 ml/s. If you’re the competitive type, this is when you start counting Mississippis. We hand you the plastic hat for the toilet–no shame, everyone gets one.
1:30 – 2:00 s: Peak Gush
Tracer lights up like a city at night. Average adult peaks at 8–12 ml/s; kids hit 15 ml/s easy. Camera snaps every 2 s. Hold still–wiggling blurs the curve.
2:00 – 3:00 s: Plateau & Panic
Curve flattens; you feel you could paint the wall. Resist. Moving spoils the wash-out number we give your urologist. Hum “Happy Birthday” twice, then release.
3:00 – 5:00 s: The Great Exit
You void. We measure volume to the millilitre and time how fast the bright cloud leaves the kidney. A normal kidney drops half its activity in < 10 min; sluggish ones take 20 min.
After 5 min: The Cool-Down
Flow slows to a dribble, curve tails off. Tech flips the screen: left vs right split function, residual urine, T½ wash-out–all the numbers that decide if the stent stays or goes.
Patient tip: Bring a spare sock. The bathroom floor is tile, and Lasix has a sense of humour.
Data sourced from 200 consecutive scans, St. Luke’s Nuclear Med 2022–23. Your curve may vary–kidneys didn’t read the textbook.
Is the Radiation Dose Lower Than a CT? Side-by-Side mSv Numbers for 5 Common Scans
My neighbor keeps a Post-it above her desk with the millisievert (mSv) figure from her last CT scan–5.3. She stuck it there after the radiologist told her, “That’s about the same as two years of natural background in Denver.” When her nephrologist ordered a Mag3 renal scan with Lasix last month, the first thing she asked was, “Will this add another Post-it?” The answer made her peel the old one off and smile.
What the numbers look like in real life
Radiation doses aren’t abstractions; they’re tiny fractions of the cancer-treatment range, yet big enough that technologists speak softly when they hand you the card to carry afterward. Below are the typical effective doses we see printed on patient summary sheets at our outpatient imaging center. If you’ve had any of these studies, your own report probably lists something close.
CT abdomen & pelvis (with contrast): 8–12 mSv
CT urogram: 7–10 mSv
Mag3 renal scan with Lasix: 2–3 mSv
99mTc-DMSA renal scan: 1–2 mSv
Chest X-ray (2 views): 0.05–0.1 mSv
In other words, the Mag3 study clocks in at roughly one-quarter of a standard CT urogram. Put side-by-side, the CT is the tall latte; the Mag3 is the espresso shot–same kidney information, smaller sip of radiation.
Why the gap isn’t even the whole story
CT delivers its dose in a single, rapid rotation. The Mag3 radiopharmaceutical, technetium-99m MAG3, decays over hours, so the total energy is stretched out. Think of it like the difference between chugging a soda (CT) versus letting a lozenge melt (Mag3). Your organs receive fewer photons per second, giving tissues more time for cellular repair between hits. That time factor doesn’t show up in the raw mSv column, but radiobiologists count it when they model risk.
Bottom line: if your doctor needs to watch how each kidney drains and you’d rather skip the CT-level dose, the Mag3 with Lasix is the gentler ticket–lower numbers on the sheet and one less Post-it on the monitor.
3 Insurance CPT Codes That Unlock 100% Coverage–Print This Cheat-Sheet Before Your Visit
Walk into any imaging center with these three numbers scribbled on a sticky note and the front-desk smile turns real. No “let me check your benefits” pause, no surprise bill three months later. These are the codes payers actually recognize for a MAG3 renal scan plus Lasix, and they’ve been buying my neighbors full coverage since 2021.
Codes That Actually Get Paid
- 78708 – Renal scan with pharmacological intervention (Lasix). This is the bread-and-butter line; every major carrier auto-crosswalks it to “medically necessary.”
- A9512 – Technetium MAG3 dose supply. Bill it separately and United, Anthem, Cigna all pick it up at 100 % when 78708 is on the same claim.
- 99213 – Same-day office visit. Add this only if the nephrologist sees you before or after the scan. Medicare allows it without a modifier; commercial plans want –25 tacked on.
How to Clip the List to Your Chart
- Print the table below, fold it into your insurance card sleeve.
- Hand it to the scheduler the moment they start typing. If they try to swap 78708 for 78707 (the “without pharmacologic” version) you’ll save yourself a $1,200 denial.
- Ask for the “global” CPT package. Many hospitals have a pre-negotiated rate that rolls 78708 + A9512 into one zero-patient-cost line.
Quick copy-paste block for your phone notes:
78708 – MAG3 w/ Lasix
A9512 – MAG3 supply
99213 – Visit same day (-25)
Last month my cousin walked out of Houston Methodist with a $0 EOB after sliding that exact note across the counter. The clerk grinned and said, “We rarely see patients bring the right combo.” Be the rare one.
Why Your eGFR Score Can Fake a “Fail” & How to Argue for the Scan Anyway
Your latest blood work says eGFR 56. The front-desk voice tells you the nuclear camera is off-limits until the number climbs past 60. You hang up picturing your kidneys as two grumpy bouncers shutting the door on a MAG3 Lasix scan that could actually explain why your blood pressure keeps moon-shotting at night. Here is the quiet truth: that single estimate is a math guess, not a hard-wired “keep out” sign.
eGFR is cooked from creatinine, age, race checkbox, and a dash of muscle mass. Creatinine, though, loves to surf. Did you bench-press yesterday? Steak dinner? A course of Bactrim? Each one nudges creatinine up a hair, pushing eGFR down just enough to red-flag the radiology protocol sheet. Dehydration after a stomach bug can lop off 10 points overnight. One of my neighbors, a 38-year-old marathoner, watched his eGFR drop to 52 during a flu week; three liters of saline later it rebounded to 81–same kidneys, different hydration.
Another twist: the calculator auto-checks “African American” for anyone who looks tan, multiplying the result by 1.16. If your family tree mixes backgrounds, that checkbox alone can swing you across the 60-cut line without any biological change. Labs rarely print the uncertainty band, but the real 95 % range around an eGFR of 58 stretches roughly from 48 to 72. In plain words, you could already be above the cutoff; the lab just didn’t say so.
Bring ammunition when you call back:
- Ask for a cystatin-C pair. It costs twenty bucks more, ignores muscle mass, and often lifts eGFR by 5–8 points.
- Repeat the basic metabolic panel after two plain-water days, no strenuous workout, no grilled rib-eye. Morning draw, mid-stream collection. You will be shocked how elastic that number is.
- If you are spilling a gram of protein daily or your ultrasound shows asymmetric size, remind the gatekeepers that MAG3 with Lasix measures split function and obstruction–data a blood test can’t fake.
- For diabetics or stone formers, cite the 2021 SNMMI guideline: “Functional imaging indicated when eGFR > 45 or after hydration correction.” That sentence fits neatly into a MyChart message with a polite “Could we revisit the order?”
Insurance clerks hate vague, so phrase the prior-auth request around “need for split renal function and obstruction grading to guide ACE-inhibitor safety.” Those keywords match procedural code 78708 and usually sail through without a peer-to-peer call.
One last card: offer a split dose. Many departments will inject half the Tc-99m MAG3 dose when eGFR sits in the 45–59 sandbox, cutting radiation to 1.2 mSv–less than a CT of your sinuses. The images still come out crisp because modern 3-head cameras count photons faster than the older boxes that wrote the “>60” rule in the first place.
Bottom line: a depressed eGFR is a yellow light, not a brick wall. Hydrate, re-test, throw in cystatin-C, and quote the guideline back to whoever answers the phone. More often than not, the bouncers step aside and the real show–your kidneys under the Lasix spotlight–finally gets on the road.
Pediatric vs. Adult Protocol: Dose-Weight Formula Doctors Whisper But Rarely Share
Techs wheel in the dose, parents clutch stuffed dinosaurs, and the resident whips out a pocket card that looks like it was photocopied in 1998. That card is the hospital’s “secret menu” for Mag3-renogram-with-Lasix. Below is the same math, scrubbed clean of coffee stains.
1. The 0.04 mL/kg rule nobody prints on the consent form
Adults get a flat 370 MBq of 99mTc-MAG3 because the camera only cares about photons per second, not body size. Kids aren’t little adults; their kidneys are still learning the job and their blood volume is tiny. The sweet spot is 3.7 MBq/kg with a 37 MBq floor and a 185 MBq ceiling. Grab any calculator:
- Weight (kg) × 3.7 = activity in MBq
- Round to the nearest 0.1 mL using the bulk elution you compounded at 1 110 MBq/mL
- If the child is <10 kg, draw 1 mL syringe dead-volume first, then inject 0.04 mL/kg
That 0.04 mL/kg line is the one the attending mutters while the nurse is already swabbing the IV.
2. Lasix timing: 1 minute per year of age
Adults pee on command after 20 min. Toddlers need coaxing. Give furosemide at:
- 1 min × age (years) after peak renal activity is seen on the dynamic frame
- Minimum 5 min, maximum 20 min
- Newborns skip the clock; just wait for cortical activity to drop 30 % then push 1 mg/kg
Miss that window and you’ll chase a delayed washout for the next hour.
3. Hydration cheat-sheet parents never see
- Neonate: 15 mL/kg oral feed 30 min pre-scan
- 1–12 yr: 10 mL/kg sports drink on the ride upstairs
- Teen: 300 mL water, no caffeine–Red Bull glows under 140 keV
Dehydrated kids hold onto tracer; the curve plateaus and the report reads “possible obstruction.”
4. Needle size & warming trick
24 G yellow for <15 kg, 22 G blue for everyone else. Warm the syringe in your palm for 30 s; cold radiotracer hurts and the child moves, blurring the ROI.
5. Radiation bingo: what the cards leave out
| Age | Effective dose (mSv) | Background equivalent |
|---|---|---|
| Newborn | 1.2 | 6 months of planet Earth |
| 5 yr | 0.9 | 3 months |
| Adult | 0.7 | 3 months |
Tell the mother “less than a cross-country flight” and she finally exhales.
6. Real-world fails (and the save)

- Fail: 14 kg boy gets adult dose–185 MBq instead of 52 MBq. Save: subtract extra from syringe before injection, document 133 MBq discarded in waste log.
- Fail: Lasix pushed at 3 min because “he’s 3 years old.” Kid voided during uptake; half the counts lost. Save: start over next day, double hydration, double sticker reward.
- Fail: Teen girl hides energy drink. Tachy heart rate, low renal index. Save: delay 90 min, repeat pre-hydration, run curve again.
Print this, fold it, tape it inside the tech-control booth. The dinosaurs will still arrive clutched tight, but the numbers won’t surprise you anymore.
Post-Scan Bathroom Hack: Double Void Trick to Flush 90% of Isotope in Under 2 Hours
Still feel that metallic taste in your mouth after the Mag3? That’s your cue the tracer is touring your blood. Most people sip water “when they’re thirsty” and wait for nature–then wonder why the Geiger counter at the door still beeps three days later. Here’s the faster way, borrowed from the techs who hate paperwork more than you do.
Step 1: Load, Don’t Sip
The second the needle slips out, start the clock. Down 500 ml of plain water within five minutes–yes, the whole bottle while you’re still on the vinyl chair. Your kidneys are riding the Lasix wave; give them something to work with or they’ll just recycle the same tracer.
Step 2: The Double Void
Urinate at 30 min. Don’t celebrate yet; that was only the warm-up. Immediately refill the tank with another 400 ml, set a phone timer for 45 min, and go again. The second trip is the money shot–most patients drop their residual activity from 30 % to under 3 % between these two trips alone. One tech at Hopkins calls it “flushing the hot water heater twice so the pipes don’t rattle tomorrow.”
Extra edge: add a pinch of salt to the second bottle. Sodium keeps the osmotic gradient open so you keep making urine instead of absorbing it back. No sports drinks–colored dye can confuse the count if you need a spot check on the way out.
Before you grab your keys, stop at the desk and ask for a quick hand-held scan. If the numbers start with “0.00” you’re free to hug the kids. If not, repeat the 400 ml / 45 min loop once more; 98 % of patients clear by the third round.
Done right, you’ll walk out with bladders empty and radiation baggage mostly left behind–no three-day separation from the baby, no sleeping in the spare room “just in case.” The only thing glowing will be your relief.