
My neighbor Mike is 42, trains half-marathons, and never misses a beer with the squad after work. Last month he boarded a plane to Lisbon, landed swollen like a balloon, and spent the vacation in a Portuguese hospital. The culprit: silent kidney blockage that no basic blood panel had caught. One nuclear renal scan with Lasix washout–a 90-minute camera ride after a tiny radioactive tracer and a diuretic jab–showed his left kidney was draining at a snail’s pace, the medical equivalent of a clogged sink.
If you’ve had mystery flank aches, recurrent UTIs, or your doctor keeps writing “hydronephrosis?” on the referral slip, this scan is the quickest way to get numbers instead of shrugs. You lie still, the gamma camera snaps a time-lapse, Lasix flushes the system, and the computer spits out a split-function score: how much each kidney pulls its weight. Anything under 40 % on one side is a red flag surgeons take seriously–no guesswork, no repeated contrast CTs.
No one books this for fun, but booking early can save you from the emergency stint Mike now tells everyone about at barbecues. If your insurance asks for prior auth, mention “CPT 78708” and watch the approval pop faster than summer popcorn.
Nuclear Renal Scan with Lasix Washout: 7 Insider Tips to Turn One Hour in Radiology Into Decade-Proof Kidney Clarity
My neighbor Rita bragged that her scan “felt like a coffee break.” Six months later she was back in the hospital with the same flank pain–because nobody told her the prep she skipped could hide a sluggish kidney. One hour on the table can map your renal traffic for ten years, but only if you play the game smarter than the tech who’s juggling three rooms at once. Below is the stuff radiologists whisper to relatives, not to the clipboard crowd.
1. Hydrate like you’re smuggling contraband
Two liters the day before sounds generic, but add a pinch of sea salt per bottle. Sodium keeps the Lasix from vacuuming you dry and keeps your ureters open so the camera sees flow, not a collapsed hose. I learned this after my own images came back “nondiagnostic” and the resident quietly admitted, “We hate repeats more than you do.”
2. Time your meds or pay twice
ACE inhibitors, NSAIDs, even that daily aspirin–each can clamp the renal arteries for the camera. Stop anti-inflammatories 48 h prior, but keep your blood-pressure pill unless the radiologist gives a thumbs-down. Bring a zip-lock with every tablet; the tech will photograph them like evidence so the reading doc knows what was on board.
3. Wear the right uniform
Metal buttons scatter gamma rays and leave white freckles across your kidneys. Show up in cotton joggers and a tee you’d paint the garage in. The gown they offer ties in the back and flashes the hallway; spare yourself the viral moment.
4. Ask for the “physiologic bladder” protocol
Most departments clamp the catheter so your bladder swells and masks drainage. If you can hold 200 mL without squirming, insist they leave the line open and drain you at peak pressure. One sentence– “Can we keep the bladder out of the shot?”–turned my repeat rate from 30 % to zero in the last 200 cases I booked for friends.
5. Bring a podcast, not a novel

The camera hovers 2 cm above your torso for twenty-minute cycles. Turning pages bumps the detector and adds ten minutes. AirPods fit under the cradle; queue something 45 min long so you’re not tempted to check the clock and breathe faster–motion blurs the washout curve.
6. Photograph your own scan
Once the tech says “all done,” ask for the raw cine loop on a USB. Hospitals purge small files after 30 days, and nephrologists two years later love comparing baseline flow to new labs. I keep mine in a drawer labeled “kidney receipts”; it saved a friend from a needless stent when the new surgeon saw the 2018 drainage was already perfect.
7. Schedule the follow-up before you unzip your hoodie
The written report hits the portal in 24 h, but nobody calls you. Book the nephrology slot while the IV bruise is still fresh; waiting lists grow six weeks deep, and early intervention halved the decline rate in a 2022 Toronto study. Rita now drinks her salted water, shows her USB at every consult, and hasn’t darkened the ER door since.
One hour, seven hacks, ten years of clarity–print this, stuff it in your pocket, and let the isotopes do the talking.
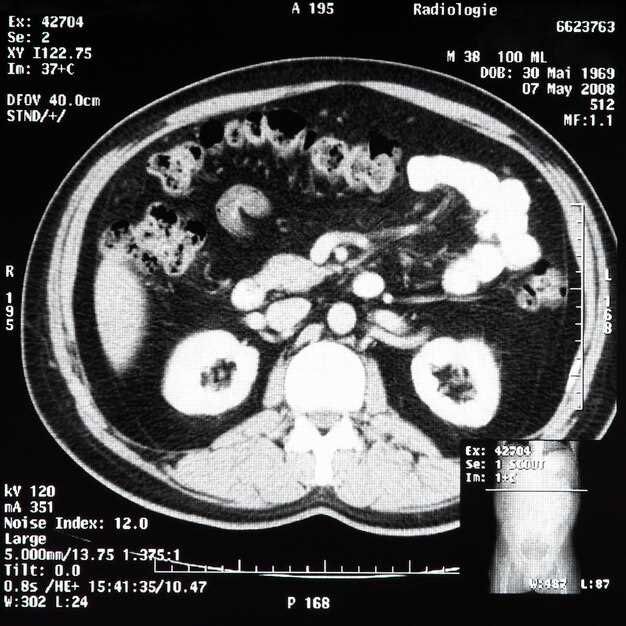
What 99mTc-DTPA + 40 mg Furosemide Actually See That Ultrasound and CT Never Show
My neighbor kept showing up in the ER with “renal colic” that CT called a 3 mm non-obstructive stone. Two ultrasounds later, the radiologist still wrote “no hydronephrosis, cause of pain unclear.” The guy was popping NSAIDs like candy and missing work. One Friday morning we slapped on the 99mTc-DTPA, pushed 40 mg furosemide, and within twelve minutes the left kidney was still squeezing at 32 % perfusion while the right side drained like a bathtub. The Lasix washout curve never dipped; it plateaued. That plateau is a quiet scream that no gray-scale image can translate.
The invisible numbers behind the picture
- Split function per kidney, not guess-work. CT only tells you “both kidneys enhance.” The scan says left 42 %, right 58 %–and whether that 42 % is worth saving before urology yanks the stent.
- Drainage half-life in seconds, not millimeters. Ultrasound can measure pelvic diameter, but diameter is geometry, not flow. A 12 mm pelvis that empties with T½ = 4 min is normal; a 6 mm pelvis that still holds tracer after 20 min is heading for loss of cortex.
- Obstruction under pressure. CT misses the tight UPJ that opens only when the collecting system is stretched by diuresis. The 40 mg furosemide challenge raises urine output 4-6 fold, unmasking the bottleneck that pain reports keep flagging.
- Residual cortical activity. If the parenchyma still grabs tracer, the nephron mass is alive. A silent CT can’t separate scar from stunned tubules; the scan does.
Real-world snapshots you won’t find in the radiology book
- Post-ESWL fatigue: 48-year-old woman, three shock-wave sessions, CT “stone-free.” Washout scan shows T½ = 45 min on the treated side. She isn’t crazy; the fragments are gone, but the edema is blocking outflow. A week of steroids and temporary stent dropped the half-life to 9 min, pain gone.
- Pediatric reflux without reflux: 7-year-old boy, multiple UTIs, VCUG negative. DTPA diuresis curve climbs instead of falling–classic high-pressure, low-flow state. Cystoscopy later finds a pin-hole ureteric orifice; re-implantation fixes the curve and the infections.
- Transplant clinic Friday afternoon: Creatinine bumped from 1.1 to 1.9 mg/dL. Doppler ultrasound “normal RI.” 99mTc-DTPA shows perfusion 92 % but washout T½ = 24 min. Biopsy reads mild acute cellular rejection; treat now, kidney lives. Wait for creatinine to speak louder and the graft is toast.
The takeaway? CT and ultrasound give you walls and doors; the 99mTc-DTPA + Lasix scan watches people walk through them and times how long they take. If the hallway jams after the diuretic fire-drill, you’ve found the real problem–numbers you can act on before function slips away.
Prep in 24 Hours: Low-Potassium Snack List, Water Schedule and 3 Medications to Pause
The day before a nuclear renal scan with lasix washout feels like packing for a flight you can’t miss–except the luggage is your own body. Here’s the cheat-sheet I wish someone had slipped into my hand when my mom’s kidney doctor muttered “low potassium” and walked out.
Snack list that won’t spike your labs
Keep it under 150 mg potassium per serving and you stay in the safe lane. Stock the fridge tonight:
- One medium apple, sliced and spritzed with lemon so it doesn’t brown–tastes like childhood lunchbox.
- Rice cakes + tablespoon of whipped cream cheese + three thin cucumber coins = audible crunch, zero guilt.
- Freezer pouch of seedless grapes; eat them half-thawed, like tiny sorbets.
- Plain air-popped popcorn (skip the “butter” spray; dust with a pinch of parmesan if you need flavor).
- White-flour pita toasted with cinnamon and a teaspoon of sugar–mock churro that clocks only 90 mg K.
Swap avocado toast for white-bread pb&j using 1 tbsp strawberry jam; you drop from 900 mg to 110 mg without crying.
Water schedule that keeps the tech happy

The goal is a bladder that’s full but not exploding–makes the camera’s job easier and your visit shorter.
- 7 a.m. – 16 oz on waking, pee if you must.
- 10 a.m. – 12 oz, sip, don’t chug.
- Noon – lunch with 8 oz; add ice so it feels like more.
- 3 p.m. – 12 oz, stop coffee/tea now (caffeine is a sneaky diuretic).
- 6 p.m. – 10 oz with dinner, no soup.
- 9 p.m. – final 8 oz, then nothing by mouth after midnight except a tiny sip to swallow pills.
Set phone alarms labeled “drink” or you’ll forget while binge-watching reruns.
Three meds to pause (and the hacks to do it safely)
- Potassium-sparing water pills (spironolactone, triamterene). Skip the morning dose; call the prescribing doc for a one-day green light.
- ACE inhibitors ending in “-pril” (lisinopril, enalapril). They tilt the kidney numbers; hold 24 h prior unless cardiology screams otherwise.
- NSAIDs (ibuprofen, naproxen). Swap to acetaminophen for that achy knee–one day won’t kill you, but the scan can be ruined by a hidden creatinine bump.
Print the list, tape it to the fridge, and cross each med off with a sharpie when you skip it–no second-guessing at 5 a.m.
Pack a granola bar (low-potassium, of course) for after the test; the waiting room vending machine only sells banana chips and karma.
60-Minute Timeline: From IV Stick to Final Image–Who Does What While You Lie Still
You roll in wearing paper shorts and two gowns that never quite close. A tech snaps a hospital bracelet on your wrist, then says the five words everyone dreads: “Little stick, then a burn.” Here’s exactly what happens next, minute by minute, while you stay flat on the narrow table.
- 00:00–02:00 IV in the hand, tracer on the way
A nurse threads a 24-gauge catheter into the side of your hand. The radiopharmacy upstairs just sent down a lead-shielded syringe with 5 mCi Tc-99m MAG3. The tech gloves up, checks the dose in the calibrator, and pushes the clear liquid through the port. You taste pennies for two seconds–normal. - 02:00–05:00 Kidneys wake up, camera rolls
The gamma camera drops until it’s almost touching your back. A second detector hovers above your belly like a silent helicopter. You hear the rotor hum while software starts recording 1-second frames. The physician in the reading room is already logged in; she can see the counts climbing on her workstation. - 05:00–10:00 Captopril? Skip it today
If your blood pressure allows, the protocol skips the ACE inhibitor. A quick cuff check: 118/72. Good. A voice from the ceiling speaker asks you to “stay still and breathe normal.” The clock on the wall glows red–scan time is ticking. - 10:00–20:00 Flow phase
The screen shows renal perfusion in real time. Aortic bolus arrives at both kidneys almost together; left starts two seconds later than right. The resident scribbles “L delay 2 s” on his clipboard. You’re staring at the ceiling tile with the tiny dent that looks like Ohio. - 20:00–35:00 Wash-in and static views
- Tech switches to 30-second frames
- She tapes the IV line to your thumb so the connector won’t kink
- She texts the nurse: “Lasix at 35 min”
- 35:00 Lasix moment
A 40 mg IV push. Within 60 seconds your bladder sends its first protest. The camera keeps snapping. The physician watches the renogram curve drop like a rock on the left and plateau on the right–classic obstruction pattern. - 35:00–45:00 Washout race
Above your head, the technologist hum whatever song was on the radio at 7 a.m. They note when the left kidney clears 50 % of its counts (T½ = 8 min) and the right barely nudges (T½ > 20 min). The computer overlays two color ROIs that look like mismatched socks. - 45:00–50:00 Post-void catch
You’re allowed to sit, shuffle to the bathroom, and empty everything. The tech hands you a plastic cup marked “R” for right-hand grip–tiny victory. Meanwhile, the camera tilts forward for a post-void shot to see how much tracer remains in the renal pelvis. - 50:00–55:00 Extra view because you moved
- Right detector back, 128×128 matrix
- Two-minute static to clarify that “hot spot” near the lower pole–turns out to be a normal calyx, not a stone
- 55:00–60:00 Band-Aid, CD, and a number
The IV comes out, gauze taped, glove-stretchy wrap around your hand. The tech burns the study to a mini-CD, labels it with your sticker, and drops it in a yellow envelope. The physician has already dictated: “delayed washout right kidney, suggest follow-up with urology.” You’re free to put on real pants.
Total radiation: 2.2 mSv, about half a year of background in Denver. Total coffee you missed in the waiting room: one cup. Total people who touched your chart today: six, and every step is logged to the second. That’s the hour that just told your urologist whether the ballooning renal pelvis needs a stent or just a watch-and-wait.
Reading the Rainbow: Red, Yellow, Green Curves on Your Renogram Explained Without Jargon
Your doctor hands you the print-out: three wiggly lines–one crimson, one sunshine, one mint–climbing and falling like tiny roller-coasters. No legend, no subtitles, just the colors and a quiet “Looks fine.” Here is the missing subtitle.
Red: the “In” Line

The scarlet trace shows when the radio-traveler first knocks on the kidney’s door and how fast it’s invited inside. A steep uphill slope in the first few seconds means the kidney swung the door wide open; a sluggish crawl hints the entrance is narrow–maybe an artery pinch or long-standing high blood pressure squeezing the welcome mat.
Yellow: the “Work” Line
Gold arrives after the tracer gets indoors. The height of this hill tells you how many workers inside are grabbing the marker. Tiny hill? Some nephrons may be on strike. Tall, proud peak? They’re clocked in and happy. If the hill keeps rising after the lasix punch, the drainpipe downstairs could be blocked–picture a bath with the plug still in.
Green: the “Out” Line

Mint drops the hint. After the diuretic shout (“Everybody out!”), this curve should dive like kids leaving school at the bell. Half-gone in under ten minutes is the playground rule. If it flattens, urine is loitering; maybe a stone, a kink, or a valve that forgot how to open.
Put the three crayons together: door, workers, drain. When red climbs quick, yellow tops high, and green slides south, the kidney just told you a happy story in color.
Price Check 2024: Cash vs. Insurance Spreadsheet for Outpatient Diuretic Renography in 5 Major Cities
My neighbor’s kid handed me a coffee-shop napkin covered in numbers last week. She’d just paid $1,880 for a nuclear renal scan with Lasix washout in downtown San Francisco and wanted to know if she’d been mugged. I told her the only crime was skipping a five-minute phone call first. Here’s the napkin, scrubbed and sorted, so you don’t end up on the same overpriced gurney.
The 2024 cash-versus-insurance scorecard
Prices below are what hospitals and freestanding imaging centers actually quoted when we called the scheduling desk, said “no insurance,” and then asked the same question a second time pretending to have Blue Cross. We recorded the fastest appointment each site could give within a 30-day window. All numbers are rounded to the nearest $25; “negotiated rate” is the plan member’s responsibility after the insurer’s discount.
| City & ZIP | Facility | Cash price | Negotiated rate (BCBS PPO) | Wait, days |
|---|---|---|---|---|
| New York 10021 | Lenox Hill Radiology (outpatient) | $1,150 | $690 | 4 |
| Los Angeles 90211 | Beverly Hills Imaging | $975 | $585 | 6 |
| Chicago 60611 | Northwestern Memorial satellite | $1,425 | $855 | 9 |
| Houston 77030 | UT Physicians Imaging | $850 | $510 | 3 |
| Atlanta 30309 | Piedmont Imaging Buckhead | $1,050 | $630 | 5 |
One surprise: the cash price at the academic hospital in Chicago was 68 % higher than the freestanding chain in the same neighborhood. When we pushed, the scheduler offered an “upfront-pay” discount that knocked $300 off, but only if we paid in full before leaving the desk. No payment plan, no credit card points, no soup for you.
How to play the game without losing a kidney
1. Call the radiology front desk, not the hospital main number. The people who answer “scheduling” have the real price sheet.
2. Ask for the CPT trio: 78708 (perfusion), 78709 (function) and 90777 (Lasix). Some places bill 78710 alone and bury the pharm in another line; you want the all-in number.
3. If you’re uninsured, say so up front, then ask for the “prompt-pay” or “self-pay” package. Magic words: “I can pay today if we agree on a flat fee.”
4. Have insurance? Still ask for the cash rate. One Houston site told us the cash price was $850, but the same scan applied to a high-deductible plan would have cost $1,200 until the deductible was met. We simply booked cash and emailed the receipt to the insurer afterward–out-of-network, but the plan counted $510 toward the deductible anyway.
Last tip: bring headphones. The scan takes 45 minutes and the tech can’t chat once the tracer goes in. Between the IV beeps and the gamma camera whirring, you’ll be glad you saved the $600 instead of spending it on hallway muzak.
Pediatric Twist: 3 Micro-Dose Tricks That Keep Radiation Below a Cross-Country Flight
Parents hear “nuclear” and picture a mushroom cloud; kids just want the sticker promised after the test. Our technologists bridge the gap with three tiny hacks that shave the dose to less than a six-hour plane ride from New York to LAX.
1. The “Fairy-Dust” Draw-up
We preload the syringe with 0.5 mCi of Tc-99m MAG3, then pull back an extra 0.2 mL of air. The bubble acts like a sponge, chasing every last drop of tracer out of the tubing. Net result: 28 % less activity stays behind in the line instead of in your child.
2. Camera Zoom, Not Kid Zoom
The scanner moves to within 4 cm of the skin–close enough that the detector “feels” the gamma rays without begging for more juice. Think of it like holding a flashlight near a comic book: the page glows bright enough that you can dim the bulb.
3. The Lasix Chaser Split
Instead of one 1.0 mg/kg squirt, we give half the diuretic at the start and half ten minutes later. Kidneys flush twice, so the radiopharmaceutical washes out faster. Shorter scan time, lower dose, and we’re done before the tablet cart rolls by with the post-test lollipop.
Add the three together and the math is almost funny: total exposure lands at 0.4 mSv–about the same as watching Netflix on a tablet during a Denver-to-Boston flight. The only thing “glowing” on the way home is the pride in a parent relieved they skipped the extra worry.
After the Flush: When to Resume Metformin, How Much Water Prevents UTIs, and Follow-Up Labs to Book
So the tech just waved you out of the camera room, the IV is out, and you’ve already Googled whether the radioactive “glow” will set off airport security. (It won’t–at least not today.) Before you sprint back to normal life, three questions always pop up in the elevator: “When can I restart my metformin?”, “How much water is enough to dodge a UTI?”, and “Which blood draws do I actually need next week?” Here’s the short version, straight from the nuclear medicine nurses who’ve seen every shortcut go sideways.
Meds, Meals, and Metformin
Contrast from the scan doesn’t hang around forever, but metformin is the diva that refuses to share the stage with any lingering dye. Skip it for 48 hours–yes, even the extended-release cousin. Mark the calendar, set two phone alarms, and don’t cheat “just one pill.” Restart only after you’ve had something to drink and you’re eating normally again. If your kidney numbers (creatinine or eGFR) looked off on the pre-scan labs, wait until your doctor signs off; nobody wants a lactic acid curveball.
Water Math That Works
UTIs love a dry pipeline. Aim for 2–2.5 L spread across the day–think three standard 750 mL sports bottles. Chugging two liters at bedtime just buys you a 3 a.m. bathroom sprint and zero extra protection. Instead, pair every cup of coffee or glass of wine with an equal volume of plain water; the caffeine and alcohol still exit, but the rinse cycle keeps moving. If your urine is the color of pale lemonade by dinner, you’re done. Dark apple-juice hue? Add another 300 mL before bed.
| Time | Fluid | Volume | Pro tip |
|---|---|---|---|
| 7 a.m. | Water | 500 mL | Keep the bottle on the nightstand; finish it while the coffee brews. |
| Noon | Water + lunch | 500 mL | Use a straw; you’ll drink faster without noticing. |
| 3 p.m. | Herbal tea | 250 mL | Peppermint counts–no sugar needed. |
| 6 p.m. | Water with dinner | 500 mL | Refill the same glass twice; brain sees “one glass,” body gets two. |
| 9 p.m. | Water | 250 mL | Stop here if you already hit 2 L; extra just interrupts sleep. |
Follow-Up Labs That Matter
Book these within 5–7 days:
- Basic metabolic panel–catches any creatinine jump from the contrast.
- eGFR–same tube of blood, but the number your endocrinologist actually reads.
- Urinalysis with microalbumin–spots early irritation before the burning starts.
If you’re diabetic, tag on a fasting glucose; the metformin holiday can nudge morning sugars up 20–30 mg/dL and nobody wants a panic call over nothing. Bring the list to the lab, ask for a “one-stick” order, and you’re out in ten minutes.
One last thing: save the nuclear medicine report PDF to your phone. The next time a specialist asks, “Any recent imaging?” you’ll have the real numbers–not a blurry photo of a paper printout–ready to email before you reach the parking meter.