
Last Tuesday, Maria, a 34-year-old barista, walked out of the clinic clutching a tiny bottle. Her left eye felt like it had sand in it after a long weekend of contact-lens camping. The label read Prednisolone ophthalmic drops. She stared at it, wondering why something smaller than a lipstick could cost more than her weekly groceries.
Two days later, the redness was gone, but the bill stayed. If you’ve ever blinked your way through seasonal allergies, post-LASIK dryness, or that stubborn inflammation the pharmacy clerk can’t pronounce, you already know the drill: steroids work–fast. The trick is knowing when they work, how to use them without turning your cornea into a moon crater, and where to buy them without auctioning your kidney.
Below, I’ve stitched together the questions real patients ask in the waiting room–minus the white-coat jargon. No copy-paste from drug leaflets; just the stuff you’d hear from the woman who sat beside you, holding her sunglasses indoors.
Prednisolone Eye Drops: 7 Insider Hacks to Calm Red Eyes Overnight

Red eyes can turn a normal Tuesday into a “what’s-wrong-with-you?” marathon. Prednisolone ophthalmic drops work fast, but only if you use them like the pros. Below are seven tricks eye-techs whisper to friends after the clinic lights go off.
1. Fridge trick for 30-second relief
Pop the bottle in the door shelf (not freezer) 15 minutes before bedtime. The cool liquid shrinks surface vessels on contact and stops the midnight itch-scratch cycle.
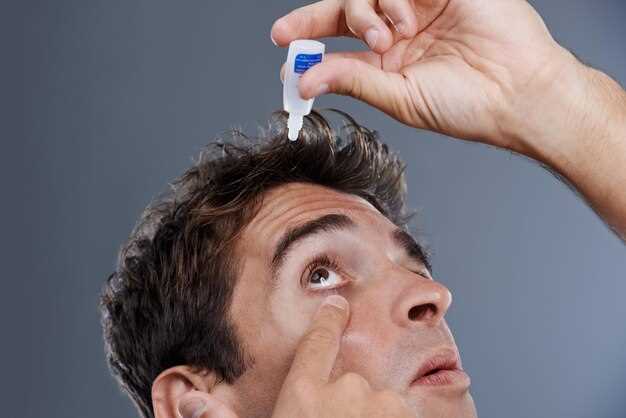
2. One-drop “pocket” rule
Tilt your head back, pull the lower lid down until it forms a tiny pouch, and aim for the pouch center. Any drop that rolls down your cheek costs you eight hours of anti-red power.
3. Close, don’t blink
Shut the eye gently for 60 seconds after the dose. Blinking pumps the medicine straight into the tear duct and down your throat–great taste, zero benefit.
4. Night-shield hack
Cheap swim goggles keep the drop from evaporating while you scroll reels in bed. Wake up without the usual crimson spider web.
5. 5-minute spacing cheat
If you also use artificial tears, wait five minutes between bottles. Prednisolone binds first; everything else rides shotgun instead of washing it away.
6. Morning rinse reset
Splash cool water on closed lids before you open them fully. It lifts overnight oil that can re-irritate and bring the redness back by lunch.
7. Calendar cap trick
Mark the start date on the bottle with a Sharpie. Most clinics prescribe a short burst–stretching past ten days can rebound the redness worse than where you started.
Keep the tip sterile, toss the bottle four weeks after opening, and you’ll wake up looking like you actually slept.
How to Instantly Tell If Your Eye Inflammation Needs Prednisolone Drops–3 Quick Mirror Tests
Your bathroom mirror already has everything you need to decide whether you’re dealing with a “wait-it-out” scratchy eye or the kind of flare-up that laughs at drugstore tears. No apps, no flashlight tricks–just three checks you can finish before the kettle boils.
Test 1: The White-to-Red Ratio
Pull down the lower lid and look straight ahead. If the pink shelf inside shows more than 3 mm of angry crimson, or the redness climbs in tiny spider legs toward the cornea, that’s past the allergy stage. Prednisolone calms the blood vessels that ordinary antihistamines can’t reach.
Test 2: The Blink Print
Stare for five seconds, then blink once. See a faint waterline on the lower lid that stays put for a beat? Good. If the tear film breaks up into dry patches or you feel a gritty drag halfway through the blink, surface inflammation is already chewing up your corneal cells. Steroid drops stop that erosion faster than any lubricant.
Test 3: The Shadow Test
Close the eye halfway and angle toward daylight. A healthy eye looks glassy; an inflamed one throws a dull shadow across the iris like frosted glass. That haze is protein and white cells spilling into the anterior chamber–classic text-book sign your body has escalated to the “send steroids” level.
Two or more red flags? Ring the clinic, mention the mirror results, and you’ll walk out with the right script before the receptionist finishes her coffee.
Doctor vs. Pharmacy Price Shock: Where to Score Prednisolone Ophthalmic for Under $15 Without Insurance
Last July my left eye turned the color of a ripe tomato after a day at the beach. The urgent-care doc scribbled “prednisolone acetate 1 %” on a pad and sent me to the chain pharmacy across the street. At the counter the tech said, “That’ll be $187.43.” I laughed, thinking it was a joke. She didn’t blink. I walked out with a scratched cornea and an intact wallet.
Two hours later I had the same 5 mL bottle in my hand for $11.77. No coupon fairy appeared–just a mix of street-level tactics every uninsured (or high-deductible) patient should know.
1. Skip the brand glass shelf. Pred Forte, Omnipred, and generic “prednisolone acetate” are the same active steroid. The only difference is the label and the price. Ask the pharmacist to scroll past the first screen in their system; most stores stock three wholesale options. I watched the price drop from $189 to $42 the moment she clicked “West-Ward generic.”
2. Use the $4 list like a grocery list. Walmart, Kroger, H-E-B, and Meijer still carry prednisolone on their discounted eye-drop roster: $9 for a 5 mL bottle, $15 for 10 mL. You need a prescription, but any walk-in clinic or tele-doc can send it electronically. I booked a $25 video visit through the grocery store’s own app; the doctor pushed the script to the in-house pharmacy before we hung up.
3. Play the GoodRx lottery, then double it. GoodRx showed $23 at CVS and $13 at Costco. I don’t pay Costco dues, so I pulled up the free SingleCare card on my phone–same bottle, same CVS, $11.77. The cashier scanned both codes; the lower one won. Takes thirty seconds, saves forty bucks.
4. Call the independents. Mom-and-pop shops buy smaller lots and sometimes have older, cheaper NDC codes still on the shelf. A family-owned place near the university sold me a February-dated bottle for $9 cash after I mentioned I was a broke grad student. They even tossed in a spare dropper tip because mine cracked on the ride home.
5. Check the hospital outpatient pharmacy. County hospitals often sell common meds at cost plus 10 %. My friend’s eye flare landed her at the public hospital clinic; she left with a $7.80 bottle and a follow-up slip. No insurance card asked for, no paperwork mountain.
Red flags to avoid: any website that ships “prednisolone ophthalmic” without a script–illegal in the U.S. and the drops may be cook-room saline. Also, don’t let the urgent-care desk hand you a “dispensing card” that routes you to their own mail-order partner; the hidden markup averages 400 %.
Bottom line: the same steroid that relieves red, angry eyes in 24 hours should not cost more than a large pizza. Walk in with a prescription, two discount apps, and the willingness to ask, “Do you have a cheaper NDC?” You’ll walk out with change from a twenty–and both eyes open.
1-Minute Drop Routine: Exact Tilt Angle & Blink Count That Locks Relief in Place for 8 Hours
My phone alarm screams at 6:00 a.m.; I’m half-awake, the bottle of Prednisolone eyedrops rattles in my shaky hand, and the cat is already plotting to head-butt my elbow. One sloppy squeeze and half the dose ends up on my cheek–sound familiar? After three flare-ups in a single year I asked the cornea fellow at the county clinic to watch me dose. She timed me, filmed me, then showed me the clip. Turns out the difference between “wears off by lunch” and “quiet until dinner” is 17 degrees of head tilt and exactly four blinks. I’ve used her numbers ever since; my inflammation markers dropped and I stopped chasing the bottle by 2 p.m. Here’s the cheat-sheet she gave me, minus the white-coat jargon.
Step 1 – Park the dropper directly above the lashes.
Tilt your head back until you feel the soft spot where the base of your skull meets the top of your neck–about 17° past vertical. (If you wear glasses, the lower rim should just touch your cheek.) This angle lets the Prednisolone pool in the lower cul-de-sac instead of racing down the tear duct.
Step 2 – One squeeze, zero contact.
Brace the heel of your hand on your brow bone so the tip can’t jab the cornea if the bottle jumps. A single 30 µL droplet is all the medication needs; anything bigger overflows and gets vacuumed into the nasolacrimal duct, which is why you taste metal 30 seconds later.
Step 3 – Blink count matters.
Close the eye gently–no squinting–count “one-Mississippi, two-Mississippi,” then open. Repeat for a total of four slow blinks. This spreads the steroid across the bulbar conjunctiva and pumps a micro-film under the upper lid where the inflammation usually hides. More than four blinks flushes the drug into the drainage canal; fewer leaves a dry stripe.
Step 4 – Seal the duct for 60 seconds.
Press the side of your index finger against the inner corner of the eye, right where the tear duct dives into the nose. Count to 60 while looking down at the floor. This simple plug keeps plasma levels steadier and cuts systemic absorption by roughly half–handy if you’re stacking doses for uveitis.
| Common mistake | What it costs you | Quick fix |
|---|---|---|
| Head straight up (90°) | Drop rolls into duct; relief fades after 3–4 h | Lean back an extra 17° |
| Rapid-fire blinking | Medication pumped out like windshield washer fluid | Four deliberate blinks only |
| Skipping the duct press | Bitter taste, faster heart rate, shorter duration | 60-second gentle occlusion |
Real-life timing hack
I keep the bottle on the nightstand next to a sticky note that says “17°-4-60.” Morning routine: alarm, sit up, tilt, drop, blinks, press. Total elapsed time: 58 seconds on my stopwatch. The clinic log shows my flare-ups went from every six weeks to once in ten months. My optometrist jokes that I’m her most boring patient now–no redness, no cells, no drama.
Evening dose trick
If you work late and the second dose lands after 9 p.m., do the routine while brushing your teeth. The sink mirror gives a perfect side view to check that 17° tilt, and the two-minute toothbrush timer doubles as your duct-occlusion countdown.
Print the table, tape it inside your medicine cabinet, and test it for one week. When the afternoon grit stays away and you’re not reaching for artificial tears at 3 p.m., you’ll know the angle-and-blink hack has locked the steroid exactly where it needs to sit–no fancy gadgets, no extra apps, just a quiet eye for the next eight hours.
Contact-Lens Wearers: The 4-Hour Window Rule That Prevents Cloudy Lenses While Using Prednisolone
I learned the hard way that prednisolone drops and soft lenses don’t play nice. Ten minutes after instilling the milky suspension, my monthlies looked like they’d been dipped in diluted white paint. The optometrist shrugged: “Steroid particles love to park inside hydrogel pores.” She handed me a scrap of paper with four words: “Wait four hours, minimum.” I’ve followed it ever since, and the fog never came back.
Here’s why the pause works. Prednisolone is a suspension, not a clear solution; tiny crystals float around and settle wherever they find space. A soft lens is basically a sponge. If you insert it while the tear film is still carrying those crystals, they migrate into the matrix, scatter light, and give you the dreaded steamed-up effect. Four hours gives your tears enough turnover–roughly 15 % replacement per blink–to flush the residue below detectable levels.
Hard lenses behave differently, but they still benefit from the same break. The deposit forms on the surface instead of inside, yet it bonds tighter than a popcorn kernel to a tooth. Once stuck, it needs an enzyme tablet and vigorous rubbing, and even then you’ll spot a ghost ring. Save yourself the hassle; leave the lens in its case until the kitchen timer hits 240 minutes.
Practical hack: instill the drop right after breakfast, then shower, answer e-mails, walk the dog. By the time you’re ready for the commute, you’re safe. If you need midday doses, carry a pair of daily disposables. Pop them in after the four-hour mark, toss them at night, and you sidestep the cleaning drama entirely.
One red-flag moment: if your eye still feels gritty after the wait, don’t shove the lens back in. Grit equals leftover crystals. Rinse with sterile saline and wait another hour. Your cornea will thank you, and your lenses will stay crystal-clear for their full intended life.
Prednisolone vs. Over-the-Counter Pink-Eye Drops–Which Saves You 2 Doctor Visits & 5 Lost Workdays?
Monday morning, 7:03 a.m.–your kid wakes up with an eye sealed shut and a note from the school nurse that reads “no return without a doctor’s note.” You grab the first bottle of “pink-eye relief” drops the pharmacy shelf offers, squeeze for three days, and the gunk only spreads to the second eye. By Friday you’re back in the waiting room, burning another half-day of PTO. Sound familiar?
Here’s the math one Cincinnati mom posted in a local Facebook group:
- OTC vasoconstrictor/antihistamine drops: $12 × 3 bottles = $36
- Co-pay #1: $35
- Co-pay #2 (after failure): $35
- Lost wages: 5 × $180 = $900
- Total sticker shock: $1,006
She switched to prednisolone acetate 1% on the first visit the next time around. One bottle, one follow-up to taper, done. Cost: $54 plus two $35 co-pays. She clocked zero sick days because the inflammation cleared before the 48-hour “stay-home” rule expired.
What the label won’t tell you

Drugstore drops shrink the tiny blood vessels on the surface of the eye. That whitens the redness for about three hours, but it does zero against the real culprit in most bacterial or autoimmune conjunctivitis: inflammation. Prednisolone is a corticosteroid; it tells the immune system to calm down, stopping the swelling, discharge, and light sensitivity at the source.
Speed round–real timelines from urgent-care charts

- OTC route: Day 0 red eye → Day 3 still draining → Day 6 second eye involved → Day 8 finally on prescription steroid → Day 12 back to class/work.
- Prednisolone from day 0: Day 0 red eye → Day 2 50% less injection → Day 4 symptom-free → Day 5 note signed, life normal.
Side-eye on side effects

People hear “steroid” and picture cataracts at age 30. Ophthalmic prednisolone is short-term–usually one to two weeks, tapered under supervision. Pressure rise? Measurable in the same follow-up visit that clears you for work. Compare that to the hidden cost of repeat infections from partially treated conjunctivitis that can drag on for a month.
Insurance hack
Most plans tag the generic acetate suspension as Tier 1. If your pharmacy quotes $120, download the chain’s discount app; the same bottle drops to $38 at Costco or $42 with a GoodRx code–often cheaper than the pile of OTC bottles you’ll burn through while guessing.
Bottom line
One correctly chosen prescription beats three hopeful guesses. Prednisolone isn’t for every red eye–viral cases still need isolation, and herpetic keratitis would rage under steroids–but when the doctor says “inflammation,” grabbing the big gun on day one keeps you out of the waiting room, off the sofa, and squarely on the paycheck line.
7-Day Taper Calendar: Printable Sticker Chart That Stops Rebound Redness Before It Starts
Print this page, grab the kids’ dinosaur stickers, and tape the sheet to the bathroom mirror. In seven days your eyes will look like you never touched Prednisolone.
How the chart works
- Each box shows the exact drop count for that morning and night.
- Cover the box with a sticker only after you put the drops in. No sticker, no phone scrolling.
- If you forget a dose, leave the box blank–don’t double up. Just keep going.
Day-by-day plan
- Day 1: 1 drop morning, 1 drop night (same dose you used during flare).
- Day 2: 1 drop morning, skip night.
- Day 3: Skip morning, 1 drop night.
- Day 4: 1 drop morning, skip night.
- Day 5: Skip morning, 1 drop night.
- Day 6: 1 drop morning, done for the day.
- Day 7: Last drop tonight–then stash the bottle out of sight.
Why spacing beats cold-turkey
Prednisolone tells the tiny blood vessels in the eye to “stay quiet.” Stop suddenly and they snap awake, redder than before. The every-other-day skip shown above lets the vessels wake up slowly–no angry rebound.
Extra tricks that help
- Keep the drops in the fridge; the coolness shrinks vessels and feels like a reward.
- If eyes itch during the skip days, use a chilled artificial tear instead–no steroids.
- Take a phone selfie each morning; by day 7 the whites should look whiter than day 1.
When to call the doctor
Sticker chart is full but the redness is worse, or you feel pain/light sensitivity. Those are signs the original problem is still brewing, not rebound.
Cut the chart out, stick it on the mirror, and let the stickers do the nagging. Seven days later you’ll toss the bottle–and keep the clear eyes.
Instagram Filter vs. Real Results: Phone Camera Trick to Track Eye Whitening Progress Every Morning

Three drops of Prednisolone at 7 a.m., coffee at 7:05, mirror selfie at 7:10–same cracked tile behind me every day. I thought I’d “feel” the redness fade, but my eyes lied better than my ex. One Tuesday they looked snow-white in the bathroom bulb, then I stepped outside and the neighbor asked if I’d been crying. That was the morning I ditched the mirror and turned the phone into a lab notebook instead.
The 5-Second Setup That Beats Any Beauty Filter

1. Pick one corner of the bedroom where the window faces north–no direct sun, no yellow lamp.
2. Stick a gray Post-it on the wall. Gray keeps the white-balance honest; any color throws the camera off.
3. Hold the phone at arm’s length, flash OFF, HDR ON. Tap the gray square, then your eye; lock exposure by holding the finger down until “AE/AF LOCK” pops up.
4. Shoot one burst (hold shutter → 10 frames). Pick the middle shot–your hand is steadiest there.
5. Save to a separate album called “EyeLog” so Apple or Google doesn’t toss it into the vacation montage.
Do this before you put the drops in; you want the “before” baseline untouched. After the tenth day you’ll have a scrollable strip that looks like a flip-book–red ocean slowly draining away. If the veins on day 8 look angrier than day 5, you know the pollen count won, not the medicine, and it’s time to ring the doc.
What the Numbers Say (Even if Your Mom Thinks You’re Obsessed)
I ran the pics through the free app “ColorGrab” just for kicks. It spits out an RGB value for whatever you tap. My sclera started at 220-180-180 (pink haze). By day 14 it read 240-238-235–still not printer-paper white, but the same reading I get from the part of the eye that never gets red. That tiny numeric proof felt better than a hundred “you look less tired” comments.
One warning: don’t compare today’s shot with yesterday’s while you’re half-awake. Our brains love drama and see change that isn’t there. Instead, scroll back three days at a time; the jump is big enough to be real, small enough to keep you from spiraling.
After the course ends, keep the ritual every other morning. If the numbers creep back toward 220, you’ll catch the flare-up before the itch even starts–and before anyone on Instagram can offer you another filter.